How to Improve Prostate Health Naturally
Tips for Prostate Gland Health
Prostate issues are nearly universal in aging men—yet few understand why this gland so often malfunctions, or what science-backed strategies can actually help. This comprehensive guide explains what's really happening with your prostate and provides evidence-based strategies to maintain optimal function throughout life.
What is the Prostate?
The prostate is a walnut-sized gland located just below the bladder, surrounding the urethra (the tube that carries urine from the bladder out of the body). As part of the male reproductive system, it serves several essential functions:
Produces approximately 30% of seminal fluid
Secretes prostatic fluid containing enzymes, zinc, and other compounds that nourish and protect sperm
Contains smooth muscle that helps expel semen during ejaculation
Helps control urination through muscular action
The prostate's unique position—encircling the urethra—explains why prostate problems often cause urinary symptoms. As the gland enlarges, it can squeeze the urethra like a clamp on a garden hose, obstructing urine flow.
Common Prostate Conditions
Men commonly experience three main types of prostate conditions:
Prostatitis
Prostatitis is inflammation of the prostate gland, often caused by infection. It affects approximately 10-15% of men at some point and can occur at any age. Symptoms include:
Pain in the genitals, groin, lower back, or pelvic area
Painful urination or ejaculation
Urgent or frequent urination
Flu-like (fever, malaise, chills) symptoms (in acute bacterial prostatitis)
Unlike other prostate conditions, prostatitis isn't age-related and typically responds well to treatment.
Benign Prostatic Hyperplasia (BPH)
BPH involves non-cancerous enlargement of the prostate gland. It affects:
8% of men in their 40s
50% of men in their 60s
80-90% of men by their 80s1
BPH causes a range of symptoms that significantly impact quality of life:
Nocturia (nighttime urination) disrupts sleep cycles for 71% of men with BPH, causing chronic sleep deprivation2
49% more men with moderate-to-severe BPH report decreased social functioning than normal men3
Sexual function declines in 72% of men with BPH4
22% report depression associated with chronic urinary symptoms5
Prostate Cancer
Prostate cancer is the second most common cancer in men worldwide. Research indicates that prostate cancer often develops in areas affected by BPH, suggesting that the chronic inflammation and cellular changes in BPH may contribute to cancer development in some cases. Key facts include:
Many men with prostate cancer will die with it, not from it
Highly treatable when caught early
Risk increases significantly with age
The Hormonal Connection: Testosterone, DHT, and the Prostate Gland Health
The prostate's health is intimately tied to hormones, particularly androgens (male hormones). Here's how the process works:
Testosterone circulates throughout the body
Within the prostate, an enzyme called 5-alpha reductase converts testosterone to dihydrotestosterone (DHT)
DHT is significantly more potent than testosterone (up to 10 times more active)
DHT binds to androgen receptors in prostate cells, stimulating growth
This hormonal pathway explains why:
BPH rarely occurs in men castrated before puberty
Drugs that inhibit 5-alpha reductase (like finasteride and dutasteride) can shrink the prostate
Vitamin D shows benefits, as it downregulates 5-alpha reductase activity
However, the hormonal explanation alone doesn't fully explain why prostate problems are almost universal in aging men, as testosterone levels typically decline with age. This paradox led researchers to investigate other mechanisms.
The Inflammation Effects of BPH
Inflammation is commonly observed in prostate tissue affected by BPH, leading many to wonder if inflammation causes BPH or results from it. Current evidence strongly suggests that inflammation is primarily a consequence of BPH rather than its cause:
BPH creates urinary retention issues, leaving residual urine in the bladder
This stagnant urine can harbor bacteria and irritants
Incomplete bladder emptying creates a reservoir that can promote bacterial growth
These factors trigger inflammatory responses in prostate tissue
Despite the presence of inflammation, attempts to treat BPH with anti-inflammatory medications have yielded disappointing results:
Non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin show no significant benefit for BPH symptoms
Antibiotics don't improve BPH unless there's a confirmed bacterial infection (prostatitis)
Antioxidant supplements targeting inflammation pathways show little benefit for BPH
The secondary effect of inflammation helps explain why so many "anti-inflammatory" dietary approaches6 and supplements fail to demonstrate significant benefits for prostate health in controlled studies. Addressing the root causes of BPH through other mechanisms (hormonal, vascular) proves more effective than targeting the secondary inflammation.
The Internal Spermatic Vein Theory
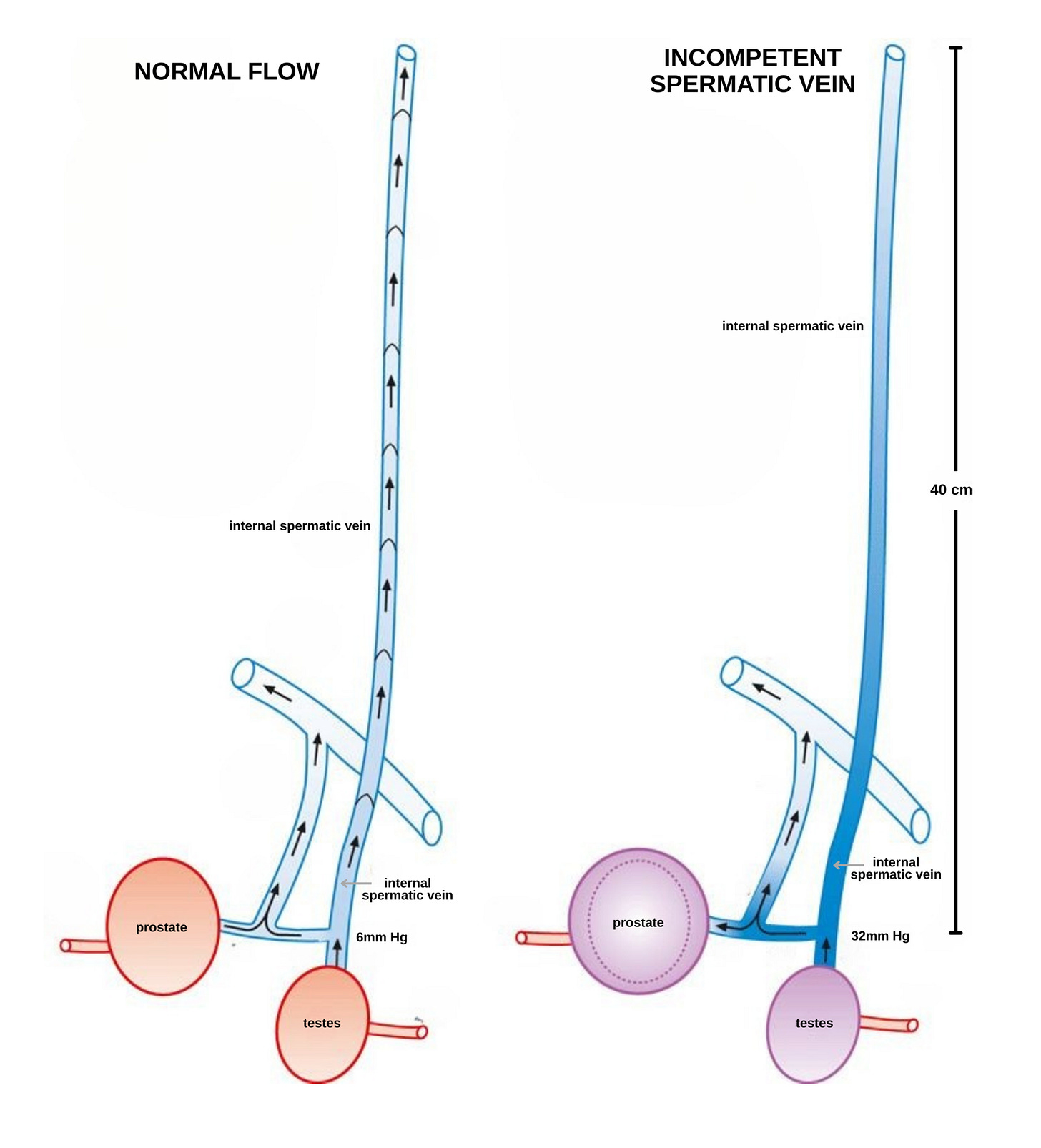
In 2005, Israeli physicians Drs. Yoram Gat and Menachem Goren proposed a groundbreaking theory that explains why the prostate enlarges with age despite declining testosterone levels. A hat tip to psychiatrist and blogger Scott Alexander, who highlighted Gat and Goren's findings7 on the connection between prostate problems and the unique vascular anatomy surrounding the prostate.
The internal spermatic veins (ISVs) drain blood from the testes and converge near the prostate before emptying into larger veins. As men age, these veins often develop incompetent valves, similar to those found in varicose veins in the legs. This creates a "backwash" effect where:
Blood pools and builds pressure in the veins surrounding the prostate
Testosterone from the testes, which would normally be diluted in the general circulation, instead bathes the prostate in concentrated hormones
This concentrated testosterone is then converted to DHT by the prostate's 5-alpha reductase
The combination of vascular pressure and high DHT exposure stimulates prostate tissue growth
This theory elegantly explains several previously puzzling observations:
Why testosterone replacement therapy doesn't increase prostate cancer risk (it replaces testicular production rather than adding to it)
Why certain exercises affect prostate health differently
Why some men with low overall testosterone still develop prostate issues
The integrity of these Internal Spermatic Veins (ISVs) can be evaluated using a standard Doppler ultrasound. Pioneering this line of inquiry, Drs. Yoram Gat and Menachem Goren developed a procedure involving embolization or ligation of incompetent ISVs, designed to correct the problematic backward blood flow. Their published clinical results were indeed striking, reporting a 34% average reduction in prostate volume and a 73% decrease in nocturia following the procedure8.However, this innovative treatment was, to the best of current knowledge (as of mid-2025), exclusively performed at their specific clinic, which now appears to be closed9. Consequently, this specific approach to treating BPH is not understood to be currently available. The reasons why such a promising procedure, performed only by its originators, did not see wider adoption or independent replication are likely complex; it's worth noting that surgical innovations, unlike pharmaceuticals, often lack patent protection, which can influence the incentives and pathways for their broader dissemination and development by others, regardless of initial efficacy. Thus, what appeared as a potentially groundbreaking treatment remains a compelling but, for now, seemingly unpursued avenue in prostate care. If any readers know about urologists or clinics offering similar procedures for BPH, please share this information in the comments section below.
How to Improve Prostate Health Naturally
Understanding the hormonal and vascular mechanisms behind prostate issues allows us to develop targeted strategies for prevention and management.
Exercise: Intensity Makes the Difference
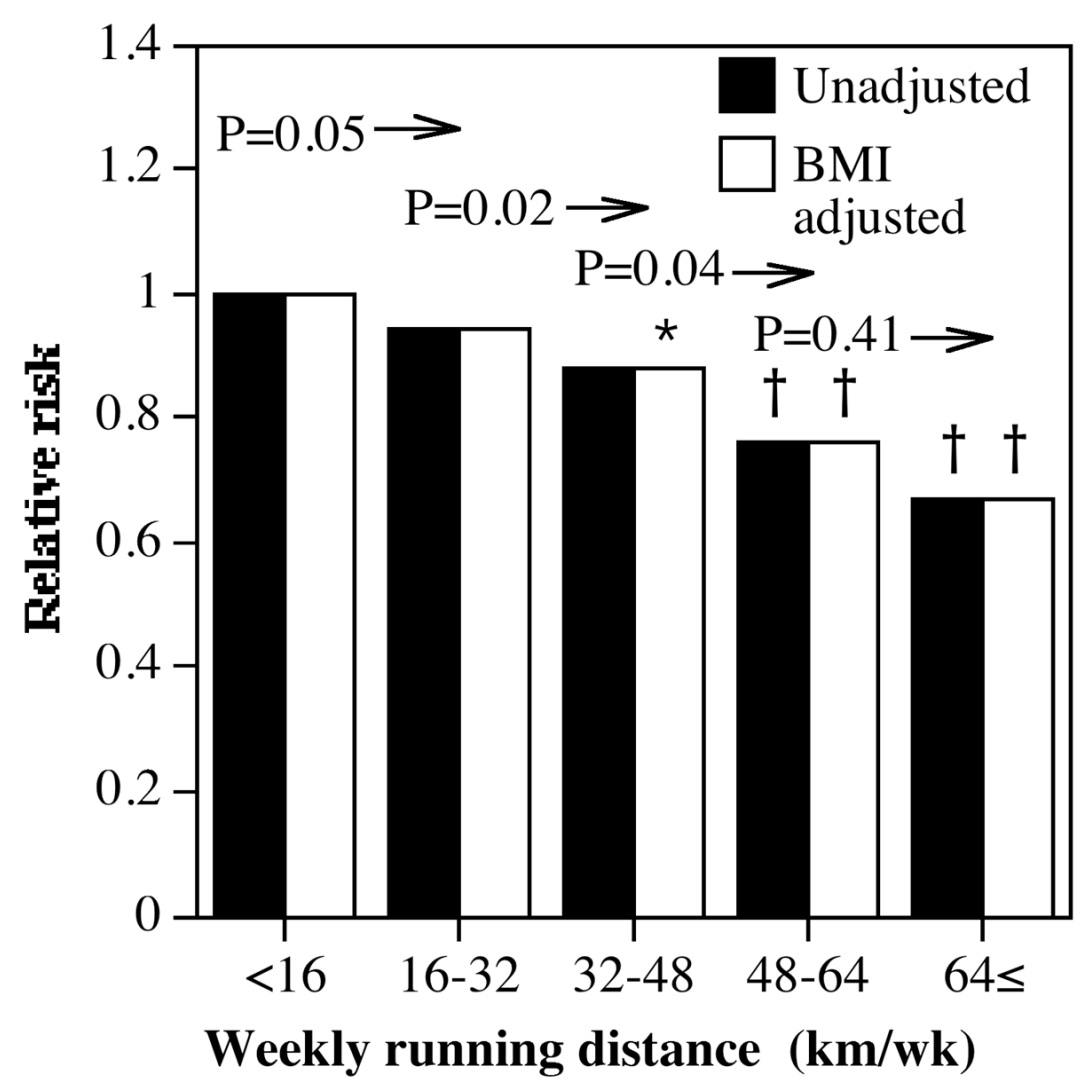
The Harvard Medical School's Health Professionals Follow-up Study—a landmark research project examining over 50,000 male health professionals—revealed that exercise intensity is the critical factor in prostate protection10:
Most Beneficial:
High-intensity activities (running, racquetball/squash): Reduce BPH risk by 14-31%
Fast walking (>4 mph): Provides 20% risk reduction compared to average pace walking
Neutral or Harmful:
Slow walking (less than 2 mph): Actually increases BPH risk by 26%
Jogging (slower than 10 min/mile pace): Shows no significant benefit despite being aerobic
Cycling: Can worsen prostate health through direct perineal pressure
The research consistently shows that intensity and volume11 matters more than the type of exercise. This perfectly aligns with the ISV theory:
High-intensity exercise increases heart rate significantly
The increased blood flow from elevated heart rate helps flush out pooled testosterone in the prostate region
This reduces the concentration of testosterone available for conversion to DHT
Lower DHT concentration means less stimulation of prostate growth
The Cycling Problem
While beneficial for cardiovascular health, cycling deserves special caution for prostate health:
The bicycle seat puts direct pressure on the perineum (area between scrotum and rectum)
This pressure can compress the prostate and surrounding blood vessels
Compression can worsen blood pooling and increase inflammation
Studies show cyclists have twice the risk of erectile dysfunction12
Cyclists training more than 8 hours weekly show significantly higher rates of prostate cancer13
For men with existing prostate conditions, consider limiting cycling or using specialized prostate-friendly saddles with cutouts.
For optimal prostate protection, aim for at least 2-3 hours weekly of higher-intensity activity that significantly elevates your heart rate. If you prefer walking, maintain a pace of at least 3 mph—slow strolling is not only ineffective but may actually increase your risk.
Diet and Prostate Health: What Really Works
Many dietary recommendations for prostate health aren't supported by robust evidence. Here's what the research shows:
Proven Beneficial Factors:
Cranberries (the best prostate food): A British Journal of Nutrition study showed a large (Hedge's g 1.6) improvement in lower urinary tract symptoms from 1.5 g of dried cranberries daily14
Moderate alcohol consumption: a meta-analysis including 120,000 men showed alcohol reduces BPH risk by 34%15
Important Caution on Alcohol:
While moderate consumption (1-2 drinks daily) appears beneficial for BPH, heavy alcohol intake significantly increases risk for prostate cancer and other cancers. Moderation is key.
Foods With Limited or No Evidence:
Dairy products: Despite common claims, meta-analyses show negligible impacts on prostate health16
Tomatoes and lycopene: Larger studies have failed to demonstrate significant benefits17
Red meat: Comprehensive meta-analyses show no clear association with prostate enlargement18
Plant-based proteins: While generally healthy, no specific evidence supports their role in prostate protection19
Best Vitamins for Prostate Health
While many supplements claim to support prostate health, few have substantial evidence. Those with the strongest scientific backing include:
Vitamin D: Strong evidence for inhibiting prostate growth through direct downregulation of 5-alpha reductase activity from 4,000 IU daily20
Cranberry extract: Several studies show improvement in lower urinary tract symptoms
Supplements with mixed or insufficient evidence include:
Zinc: Despite the prostate containing high zinc levels, supplementation shows inconsistent results21
Saw palmetto: Early promising results haven't been consistently replicated in larger studies
The evidence is clear: despite numerous claims about prostate-friendly foods, only vitamin D, moderate alcohol consumption, and cranberry products have shown meaningful benefits in meta-analyses. Most lack compelling evidence specifically for prostate health. Focus on the few proven factors rather than overhauling your entire diet.
Medication Options When Needed
For men already experiencing symptoms, certain medications provide effective relief:
Tadalafil (Cialis): Dual Benefits for BPH and Sexual Function
Originally developed for erectile dysfunction, tadalafil at 5mg daily was FDA-approved for BPH treatment in 2011. Clinical research shows it:
Reduces BPH symptoms significantly within 4-12 weeks
Improves erectile function simultaneously
Shows fewer sexual side effects than other BPH medications
Works by relaxing smooth muscles in the bladder and prostate

Other Medication Options
Alpha-blockers (tamsulosin/Flomax): Provide quick symptom relief but don't alter disease progression
5-alpha reductase inhibitors (finasteride, dutasteride): Actually shrink the prostate over time by blocking testosterone conversion to DHT but may cause sexual side effects
Prostate Testing and Screening
PSA (Prostate-Specific Antigen) testing has been widely promoted, but its value is frequently misunderstood. While PSA can detect prostate cancer, it's important to recognize its significant limitations. Elevated PSA levels can result from many non-cancerous conditions:
BPH (benign enlargement)
Prostatitis (inflammation)
Recent ejaculation or digital rectal examination
Vigorous exercise, especially cycling
Current Guidelines
The United States Preventive Services Task Force (USPSTF) recommends against routine testing for most men:
Ages 55-69: PSA testing is generally not recommended unless you have specific risk factors (family history, African American heritage)
Age 70+: Routine PSA screening is not recommended
These evidence-based guidelines reflect research showing that for most men, the harms of testing (false positives, unnecessary procedures, treatment complications) outweigh the small potential benefits.
If You Decide to Test
For men with risk factors who choose to test after discussion with their doctor:
Avoid cycling for 24-48 hours before testing22
Avoid running or vigorous exercise for 24 hours before testing
Avoid ejaculation for 24-48 hours before the test
Postpone testing if you have a urinary tract infection or prostatitis
Remember that even with these precautions, PSA testing remains an imperfect screening tool with significant limitations.
Your Complete Prostate Protection Plan
Based on the evidence, here's your action plan for optimal prostate health:
Exercise with intensity: Incorporate at least 2-3 hours weekly of higher-intensity activities
Walk briskly: If walking is your preferred exercise, maintain a pace of at least 3-4 mph
Optimize vitamin D: Through sensible sun exposure or supplementation
Consider moderate alcohol: If you drink, 1-2 drinks daily appears beneficial
Try cranberries or extract: For symptom management
Consider tadalafil: If experiencing both urinary symptoms and erectile difficulties
Prostate problems may be common with age, but they're not inevitable. By understanding the vascular mechanisms underlying prostate enlargement and implementing these evidence-based strategies, you can significantly reduce your risk and maintain optimal prostate function throughout life.